Stubbing a toe is a painful injury that can vary in severity, depending on the structures involved. The lesser toes, which each contain three small bones called phalanges, are held together by ligaments and moved by tendons during walking. When the foot collides with a solid object, the result may range from a simple bruise to a more complex injury. A mild stubbed toe usually causes bruising or minor ligament strain, leading to temporary swelling and discomfort but no long-term damage. More severely stubbed toes include fractures of the bones or significant ligament injury, which can cause prolonged pain, swelling, and stiffness. In rare but serious cases, a stubbed toe may involve a dislocated joint, an open fracture where bone pierces the skin, or an angular deformity that requires surgery to correct alignment. A podiatrist can evaluate the injury, confirm its severity, and provide the appropriate treatment. If you have stubbed your toe, it is suggested that you make an appointment with a podiatrist for treatment options.
Toe pain can disrupt your daily activities. If you have any concerns, contact one of our podiatrists of Carolina Foot & Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
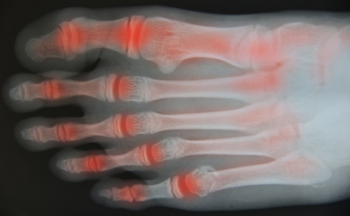
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please contact our offices located in Mount Pleasant and Charleston, SC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.