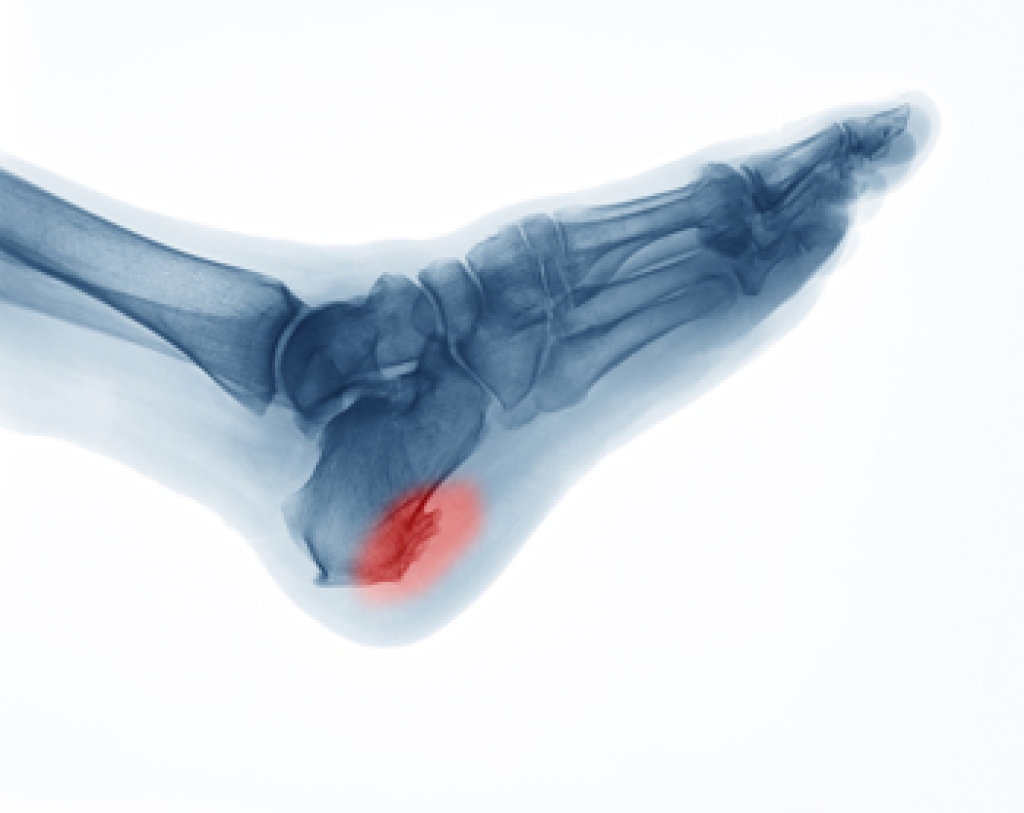
 The age group of people who are typically affected by Sever’s disease is between ten and fourteen. It impacts the growth plate in the heel and can cause severe pain and discomfort. It can happen as a result of participating in running and jumping activities, which can exert excess pressure on the heel. It is beneficial to perform stretches that can loosen the Achilles tendon which is connected to the heel. Additionally, many patients wear specific types of footwear that can help in the healing process. If you notice your child is limping or complaining of heel pain, it is strongly suggested that you schedule an appointment with a podiatrist who can diagnose and treat Sever’s disease.
The age group of people who are typically affected by Sever’s disease is between ten and fourteen. It impacts the growth plate in the heel and can cause severe pain and discomfort. It can happen as a result of participating in running and jumping activities, which can exert excess pressure on the heel. It is beneficial to perform stretches that can loosen the Achilles tendon which is connected to the heel. Additionally, many patients wear specific types of footwear that can help in the healing process. If you notice your child is limping or complaining of heel pain, it is strongly suggested that you schedule an appointment with a podiatrist who can diagnose and treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see one of our podiatrists from Carolina Foot & Ankle Specialists. Our doctors can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Mount Pleasant and Charleston, SC . We offer the newest diagnostic and treatment technologies for all your foot care needs.